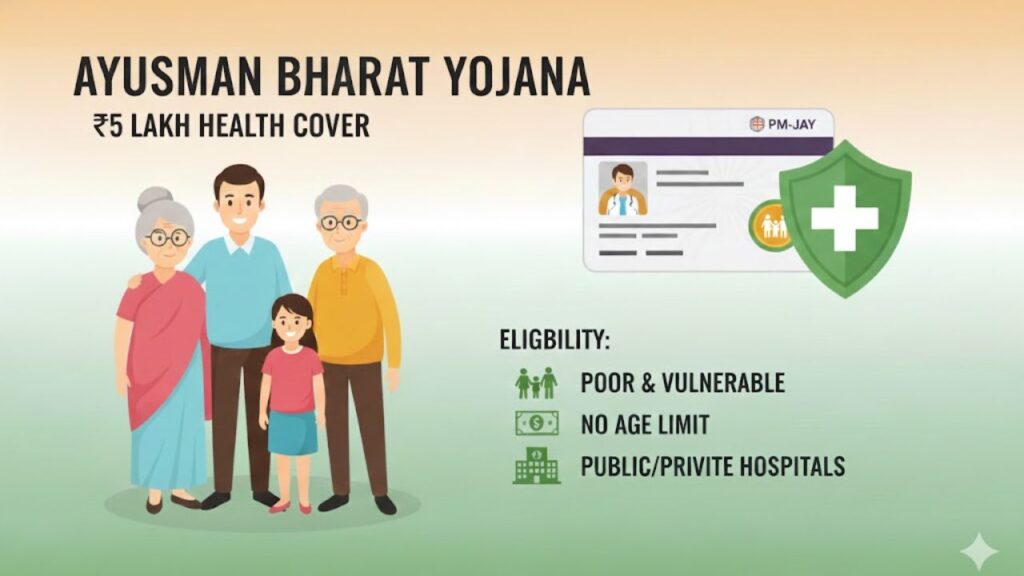
A strong nation is built on the health of its people. To make quality healthcare affordable and accessible for everyone, especially poor and vulnerable families, the Government of India launched a large-scale health insurance programme known as Pradhan Mantri Ayushman Bharat Yojana.
This scheme focuses on providing cashless treatment for serious medical needs so that families do not fall into debt due to hospital expenses. Below is a complete and clearly explained guide covering eligibility, benefits, hospital criteria, senior citizen coverage, and the registration process.
⭐ What is Pradhan Mantri Ayushman Bharat Yojana (PM-JAY)?
Pradhan Mantri Ayushman Bharat Yojana is a government-funded health insurance scheme that provides medical cover of up to ₹5 lakh per family per year. The coverage is offered on a family floater basis, meaning the entire family can use the insured amount.
Earlier known as AB-NHPS, the scheme is now officially called Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY). It has replaced earlier health schemes like Rashtriya Swasthya Bima Yojana and senior citizen health insurance programmes.
⭐ Key Features and Benefits of Ayushman Bharat Yojana
- Health insurance cover of up to ₹5 lakh per year per family
- Covers primary, secondary, and tertiary healthcare
- Cashless treatment at government and empanelled private hospitals
- Covers pre-hospitalisation and post-hospitalisation expenses
- Includes daycare procedures
- All pre-existing diseases are covered
- Follow-up treatment expenses up to 15 days included
- No cap on family size, age, or gender
- Targets nearly 40% of India’s population (poor and vulnerable families)
- Entire treatment cost during hospitalisation is covered
⭐ Eligibility for Ayushman Bharat Yojana – Rural Families
Rural households are identified based on Socio-Economic Caste Census (SECC) 2011 data. A family is eligible if it falls under any of the following categories:
- Families with no adult member (16–59 years)
- Female-headed households with no adult male member
- Families living in single-room houses with kutcha walls and roof
- Households belonging to Scheduled Castes (SC) or Scheduled Tribes (ST)
- Families with disabled members and no able-bodied adult
- Landless households earning from manual casual labour
Automatically Eligible Rural Categories
- Destitute families dependent on alms
- Manual scavenger families
- Bonded labour families
- Particularly Vulnerable Tribal Groups (PVTGs)
⭐ Eligibility for Ayushman Bharat Yojana – Urban Families
Urban eligibility is based on occupation, not income. A family must belong to one of the following occupational groups:
- Street vendors, hawkers, cobblers
- Domestic workers
- Rag pickers and beggars
- Construction workers, plumbers, masons, painters, welders
- Coolies and head-load workers
- Sweepers, sanitation workers, gardeners
- Transport workers (drivers, conductors, cart pullers)
- Artisans, handicraft workers, home-based workers
- Washermen and watchmen
- Electricians, mechanics, repair workers
- Peons, helpers, shop staff, delivery assistants, waiters
⭐ Special Coverage for Senior Citizens (70+ Years)
On 11 September 2024, the Union Cabinet approved universal coverage for all senior citizens aged 70 years and above, regardless of income or socio-economic status.
Key Points for Senior Citizens
- All citizens aged 70+ years are eligible
- Separate Ayushman Card issued for senior citizens
- Eligible families already covered under PM-JAY receive an additional ₹5 lakh top-up
- This senior citizen cover is separate from family coverage
If Already Covered Under Other Schemes
- Seniors covered under CGHS, ECHS, or CAPF schemes can choose either PM-JAY or their existing scheme
- Seniors with private health insurance or ESI can also avail PM-JAY benefits
⭐ Eligibility Criteria for Hospitals Under PM-JAY
Hospitals must meet strict requirements to be empanelled:
- Registered with State Health Agency
- Minimum 10 inpatient beds
- 24/7 availability of qualified doctors and nurses
- Functional washrooms and sanitation facilities
- Interoperable IT system for patient data
- Dedicated medical officer for PM-JAY
- Ambulance and emergency services
- Nearby blood bank and diagnostic lab
- Proper electricity, water supply, and biomedical waste disposal
⭐ How to Register for Ayushman Bharat Yojana Online
Follow these steps to check eligibility and register:
- Visit the official PM-JAY portal
- Enter your mobile number and captcha
- Click on Generate OTP and verify
- Select your state
- Search eligibility using:
- Mobile number
- Name
- Ration card number
- RSBY URN number
If eligible, your name and family details will appear on the screen.
⭐ How to Claim Cashless Treatment Under PM-JAY
- Eligible families receive an enrolment letter with QR code
- Empanelled hospitals have an Ayushman Mitra
- QR code is scanned to verify eligibility
- After ID verification, a Golden Card is issued
- Treatment is provided cashless
- Government hospitals are automatically empanelled
Conclusion
The Pradhan Mantri Ayushman Bharat Yojana is one of the world’s largest public health insurance schemes, offering ₹5 lakh annual coverage to millions of families. With wide eligibility, senior citizen inclusion, and cashless treatment facilities, it plays a major role in protecting families from financial stress caused by medical emergencies. For simple, step-by-step guidance on Ayushman Bharat, health cards, and other government schemes, visit Sarkari Bakery.